Why UAB Women & Infants Center?
Advanced Maternal Age
I chose UAB because it is known for its world-class care and the physicians are top-notch. I didn’t get married until I was 35, and by the time I had babies, I was considered Advanced Maternal Age (AMA). Having a high-risk Maternal Fetal Medicine (MFM) clinic in-house was important.
Proximity to the NICU & Children’s Hospital
Birth Plan Flexibility
I knew that I wanted a doctor that was completely on board with a natural childbirth and would allow me to be included in my plan of care. My doctor, Kim Hoover, M.D., guided me through all three pregnancies. She allowed me to go into my first delivery (in 2016) as I wished. I was allowed to labor with a birthing ball, a peanut ball, in the shower, in multiple positions with intermittent monitoring, and only a Hep-lock.
Unfortunately, after 47 hours of laboring, both at home and at the hospital, my son’s heart rate dropped, he had meconium, and I developed a fever. By this time, shifts had changed multiple times and the new on-call doctor allowed me to collaborate with him to develop a new plan of care that included a Cesarean.
Second Time Around
As the pregnancy came to an end, my cervix never changed and was once again not favorable to deliver vaginally. As we went into the Cesarean, we were surprised to find that I had developed uterine adhesion disease. The procedure took much longer than expected, but in the end, my baby girl and I came out healthy and happy.
Third Time’s a Charm
Being the overachieving patient that I am, we had a surprise a few months after delivering: we were pregnant again. This time (June 2019) we knew going into the pregnancy that I would need a Cesarean and that it would be more in depth than the previous two. It would be difficult not only because of the adhesion disease, but I would also be delivering only 12 months after my last surgery. Keeping in mind that any surgery causes scarring and I now had a history of excessive scar tissue times two, we prepared to be in the surgery suite longer than the typical procedure time.
I knew that a spinal only lasts a couple of hours and we would risk going over that time frame. We originally opted for an epidural. The morning of my daughter’s birth, I arrived early to be prepped for surgery. The attending anesthesia physician made a point to come to my room and discuss the case outside of the typical visit from other anesthesia staff doctors. He, like the others, wanted to include me in the plan of care. With my first two pregnancies, the morphine caused me to itch postpartum, so we opted to use less this go around. It worked: I didn’t itch at all this time. We opted to do a spinal while also placing an epidural catheter. That way we could go the easier route of a spinal in case the procedure didn’t last as long, but still have the epidural catheter in place in case we needed to dose it for a longer procedure.

Convenience and Parking
The Women & Infants Center is a freestanding building that is connected to the rest of the hospital via crosswalks, and it is very easy to navigate. Parking can be found in multiple places: under the building, outside in a paid lot, and in a deck through the North Pavilion of the hospital.
While many people may find UAB intimidating, this building is very accessible. The Maternity Evaluation Unit, Labor and Delivery, the OR suites, recovery, the postpartum unit, High Risk Obstetrics, the physicians’ offices, Maternal Fetal Medicine, and the Regional NICU are all in the same building.
The Rooms
The typical suite is nice and spacious: it has a sofa that converts into a bed for your spouse, space for multiple bassinets if needed, plus room for many guests. UAB is set up so you are moved to a postpartum room after recovery. I really liked this and would choose it time and time again, because it made for a much quieter recovery for myself, my husband, and our baby.
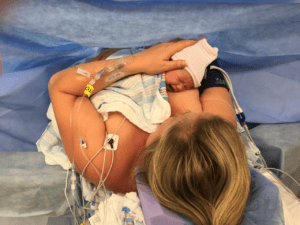
Lactation Help
I have chosen to breastfeed all my children, and they each have been very different. The lactation consultants at the UAB Women & Infants Center have gone above and beyond every time. They visit every day and are on call if you need them.
My first baby had a four-day NICU stay and didn’t latch well after birth. Lactation spent hours with me ensuring that he was able to latch and I was comfortable before we went home. They helped me with nipple shields, teaching me different holds, and different ways to encourage and strengthen his latch.

As stated earlier, my second pregnancy was a gestational diabetic (GDM) pregnancy. I was concerned about my baby’s blood sugar levels being too low after birth so I hand expressed colostrum and froze it in syringes before delivery. The NICU stored the colostrum, and though her glucose levels were perfect, we had it on hand just in case. Lactation was there with me every step of the way and even called to check in for the first six months of our breastfeeding journey.
With my third baby, my daughter made an odd clicking sound with every feed. Lactation, once again, was there in minutes. The lactation nurse watched and listened before telling me she saw no tongue ties, no lip ties, or anything wrong. She encouraged me that my daughter was still learning how to nurse and that it would more than likely go away within 24 hours. Sure enough, it did.
And That’s Not All!
In addition to the amazing amenities, care, and expertise we experienced at UAB, every couple that delivers there is given a celebratory steak dinner with sides, dessert, and sparkling grape juice. How’s that for service?!