January is officially Thyroid Health Awareness Month, and as someone who recently had a thyroidectomy, I wanted to share some information from Dr. Brenessa Lindeman at UAB/Kirklin Clinic, who performed my surgery in September of 2021.
January is officially Thyroid Health Awareness Month, and as someone who recently had a thyroidectomy, I wanted to share some information from Dr. Brenessa Lindeman at UAB/Kirklin Clinic, who performed my surgery in September of 2021.
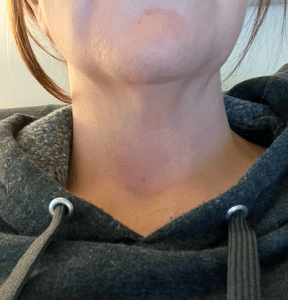
I have shared my story in a previous blog post, but I wanted to ask Dr. Lindeman some general questions regarding what women need to know about this butterfly-shaped gland that sits low on the front of the neck.
Question: What are common thyroid issues and at what age do they most often affect women?
Answer: It is estimated that one in eight women will have some type of thyroid disorder over the course of her life. Most of these are problems with hormone function, and they can range from alterations of the thyroid hormone levels (hypothyroidism or hyperthyroidism) to cancer. Thyroid hormone disorders increase in prevalence with age, and can range from three to 16 percent of people over 60.
Thyroid cancer is most common in individuals 20-55 years of age. It is estimated that one to two percent of people will have thyroid cancer at some point in their life. It affects women two to three times more frequently men.
Q: What are some signs and symptoms women experience that are related to thyroid issues?
A: Because our thyroid gland controls metabolism, most problems with thyroid hormones can make you feel tired or sluggish. When your levels are too low, you may feel cold when others do not, have constipation, gain weight despite not eating more food, and have dry skin and hair. When thyroid levels are too high, symptoms are typically the opposite, such as feeling warm when others do not, hyperactive bowels/diarrhea, losing weight without trying, feelings anxious, and experiencing tremors and/or heart palpitations.
There are a few symptoms related to thyroid nodules that may contain cancer. These include a visible neck bulge, sensation of neck pressure, or difficulty swallowing.
Q: How do I know if my problems are thyroid related?
A: The first step in investigating any potential thyroid problem is thyroid hormone testing. This can help diagnose any abnormality in thyroid hormone levels. If a nodule is suspected or has been identified in the thyroid gland, ultrasound imaging is typically the next step.
Q: When should I get it checked out?
A: You should contact your doctor if you experience any of the symptoms listed above, as a simple blood draw is all that’s needed to check thyroid hormone levels. Your doctor can also examine your thyroid and determine if other imaging, such as an ultrasound, is needed. Most patients will want to start with their primary care provider to ensure that their problems are truly thyroid-related. Because the thyroid plays into so many of our body’s functions, sometimes the symptoms can be masked by other conditions.
Q: Are many thyroid problems found incidentally as mine were?
A: Most thyroid hormone disorders are identified because patients have symptoms that affect their quality of life. Thyroid nodules, by contrast, are most often found incidentally on imaging performed for other reasons. Only four to seven percent of thyroid nodules can be felt on an exam, but anywhere from 19-67% of the general population can be found to have a thyroid nodule on an ultrasound exam, incidentally.
Q: Are thyroid nodules common? When is surgery recommended and when can they just be monitored?
A: Thyroid nodules are very common. About 19-67% of the population will be found to have at least one nodule on a neck ultrasound. But despite how common they are, only about five percent will turn out to be cancerous. So, trying to determine whether cancer is present is very important to avoid unnecessary testing or surgery.
The characteristics of a nodule on the ultrasound are used to determine whether or not a biopsy should be performed. (Nodules can be solid or cystic, or they may have calcification, etc.) Results of the biopsy are then used to determine next steps, which may include other testing or surgery.
Size is also important! It is recommended that all nodules smaller than four centimeters in size be removed because biopsies become less reliable at that size.
Q: So if you have to have surgery, what is the process of a thyroidectomy and the recovery time?

A: There is often much misinformation on the internet about this! At UAB, thyroidectomy is an outpatient procedure, whether we are removing half of the thyroid or the whole thing. Surgery takes anywhere from one to two-and-a-half hours, but patients need to block out their whole day to include a couple of hours before surgery and at least two hours in recovery.
Surgery is done through a small (typically one- to two-inch) incision located on the front of the neck and hidden as best we can in a natural neck crease. Risks of thyroid surgery are small (only around one percent have complications), but include bleeding and hoarseness or voice changes. Low calcium can be a problem after removing the entire thyroid due to irritation of the nearby parathyroid glands. However, most patients only need to take calcium supplements for a few weeks after surgery.
There are no stitches or staples to be removed after surgery because the incision is covered in a surgical super glue that falls off on its own in a couple of weeks. Recovery typically involves a very sore throat for two or three days and afternoon fatigue for one or two weeks. Most patients have very little pain which can be managed with acetaminophen (Tylenol) or ibuprofen (Advil, Motrin).
Q: Will I have to take medications after surgery?
A: Thyroid function is essential for life, so taking thyroid hormone replacement is mandatory after removal of the entire thyroid gland. In the same way that our body has duplicate function in other organ systems, one-half of the thyroid can typically take over function of the whole. Most studies show that around 75% of patients that have normal thyroid function going into surgery and have only half removed won’t need to take thyroid hormone replacement medication. This estimate lasts for approximately the first five years after surgery, because the likelihood of hypothyroidism generally increases with age. Additionally, patients with a history of thyroid inflammation or a family history of thyroid dysfunction are more likely to need thyroid hormone replacement medication sooner.
*One more important note: there is often more than one acceptable strategy for management of a thyroid nodule or cancer. Treatment decisions should be individualized for each patient after discussion with their surgeon or physician. New scar-less techniques to shrink benign thyroid nodules are now being offered at UAB for patients that meet specific criteria.